- India
- International
Why indigenous HPV vaccine has the potential to drastically bring down the incidence & deaths caused by cervical cancer in India?
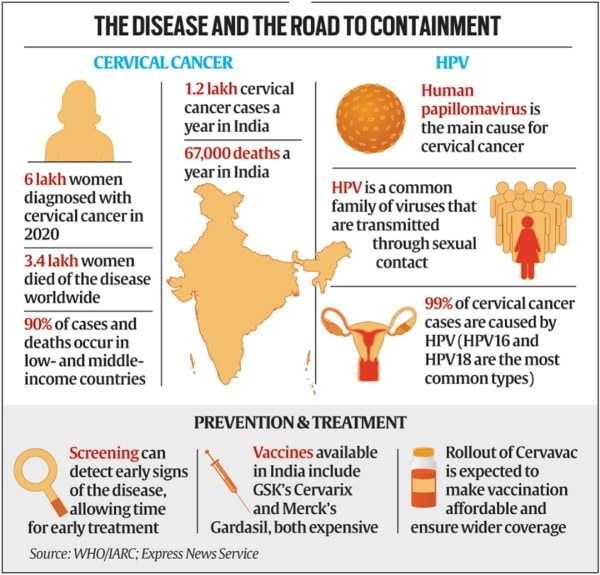
India in the next few months will have an indigenously developed human papilloma virus (HPV) vaccine --- Cervavac --- that will offer protection against cervical cancer, the second largest killer among cancers in women.
 Now, Cervarix is not readily available in India so we had to start using the other one, which is costlier, says Dr Kishore Singh.
Now, Cervarix is not readily available in India so we had to start using the other one, which is costlier, says Dr Kishore Singh. Dr Kishore Singh tells Anonna Dutt that with a cheaper, indigenously developed vaccine against HPV soon to become available, routine immunisation of all girl children would be extremely cost-effective ——and may in the coming years drastically bring down the rates of the resulting cervical cancer.
Why Dr Kishore Singh: Dr Singh, a radiation oncologist by training, currently heads Delhi government’s only standalone cancer treatment centre Delhi State Cancer Institute. The institute, currently, runs the country’s only public HPV vaccination programme for school children.
First of all, how does vaccination against an infection protect against cancer?
Cervical cancer continues to be one of the only vaccine-preventable cancers. If you see, almost all cervical cancers are found in women who have a history of HPV infection. This is not to say all HPV infections can lead to cancer; not at all. In fact, over 80% of women have an HPV infection in their lifetime and almost all of them can clear it. But in some people some high-risk types of HPV persist and lead to cervical cancer. In addition, having multiple sexual partners, poor hygiene, smoking are other factors that increase the risk of developing cervical cancer.
So, the best way to prevent the cancer is to prevent an infection in the first place. And, that is what the HPV vaccines do. There are two to four types of HPV that lead to almost 70% to 80% of all the cervical cancers and the vaccines prevent these infections. Since the virus is sexually transmitted, it has to be given to teenage girls before they are sexually active. Once an infection happens, the vaccine cannot clear it out. Hence, the effectiveness of the vaccine keeps dropping with age.

India’s first quadrivalent HPV vaccine manufactured by SII has received a regulatory approval. How will the new vaccine help?
At present, there are two HPV vaccines available – GSKs Cervarix and Merck’s Gardasil. The first one protects against the two most common types HPV 16 and 18, whereas the second one protects against two additional types 6 and 11. Now, these vaccines cost between Rs 2,500 and Rs 3,300 per dose, with teenagers requiring at least two doses and those getting it later in life needing three.
The problem then is a universal immunisation of all teenage girls becomes an expensive proposition. Yet, Delhi government in 2016 took the decision to start the immunising school girls at DSCI. The programme was halted for two years during the pandemic mainly because of two reasons. One, not many people were coming to the hospital to get a shot. Two, we were unsure on what the immune response would be like in children who might have a current infection or one recently.
Now, Cervarix is not readily available in India so we had to start using the other one, which is costlier. When we started the tendering process for a fresh batch of vaccines, we realised that the India-made vaccine will soon be available. And, this is the role the new vaccine will play. It will make it cheaper and more cost-effective for governments to give the shot under public health programmes.
And, hopefully it will become a part of the national programme as well.
What will be the impact of a universal vaccination programme? And, why did it not take off till now?
The impact will be tremendous if we are able to vaccinate 90% of the teenage girls. It will drastically bring down the incidence and deaths caused by cervical cancer in India, which is more important considering the fact that the country contributes to about a fourth of the global mortality from cervical cancer. India sees about 1.2 lakh cervical cancer cases a year and around 67,000 deaths a year. Even without vaccination the incidence and deaths due to cervical cancers are declining in India and globally – it has moved down to the second position after breast cancer from being the biggest killer among cancers in women in India – but the vaccine wipes out more than two-thirds of the cases and deaths that are caused by the four most common types of HPV.
The vaccine must be given to children starting at about age 12 to 16 years. It can be taken up to 26 years but then a third dose is needed and the vaccine is not as effective because the exposure might already have happened.
Even though we have known about the effects of vaccination – and there were previous discussions the government had about including it as a part of the national immunisation effort – it did not happen because of the unfortunate incidence Andhra Pradesh and Gujarat. There were procedural lapses in conducting the trial there which led to the news linking the vaccine to some of deaths in trial participants. This led to the government taking a back-foot.
Globally, we have seen that HPV vaccine is very safe and effective. There is a minuscule chance that a person has an adverse effect, which is true of any vaccine.
For those who have missed the window of opportunity to get the vaccine, how can cervical cancer be prevented?
For those who are past the age of HPV vaccination, regular screening is the best way to keep an eye out for whether they have cervical cancer. Earlier, we used to do a pap smear (a procedure where a small brush is used to remove cells from the cervix to be studies under a microscope) we now perform an HPV test. The sample is collected in a similar manner but it looks for the high-risk types HPV in the cells.
This test should be done starting two to three years after sexual activity begins, then every five years till the age of 65 years.
In fact, the government has already prepared a module for screening of the cervix – along with the oral cavity and breast – at the health and wellness centres so that the cancers can be detected at the earliest.
More Lifestyle
Apr 18: Latest News
- 01
- 02
- 03
- 04
- 05